Members wanted for Public Advisory Group
Become a patient and public involvement contributor!
For more details, please contact us here, we would love to hear from you.

- Have you had Hepatoblastoma (HB)
- Do you care for someone with Hepatoblastoma (HB) and/or Hepatocellular Carcinoma (HCC)?
- Do you work in the voluntary sector with people who experience Hepatoblastoma (HB) and/or Hepatocellular Carcinoma (HCC)?
- Could you help us to improve the research that we are doing into HB and HCC
This will involve you in attending our external advisory board meetings, twice a year here in the UK or in one of our Beneficiaries location in Europe.
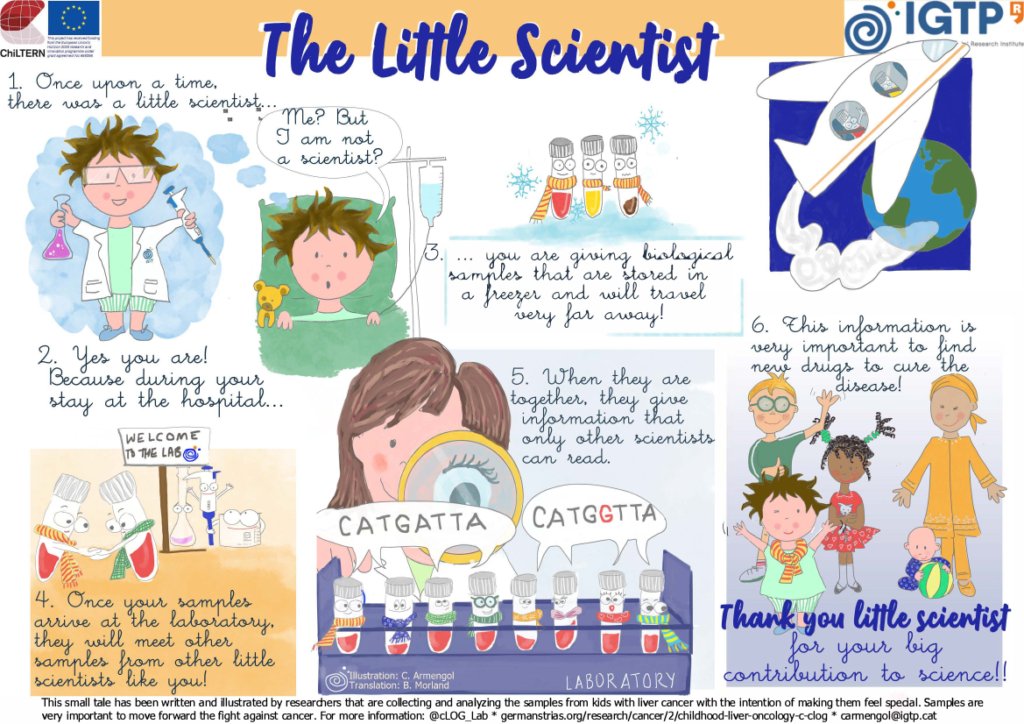
The Little Scientist and importance of samples collection
The poster below has been written and designed by researchers that are collecting and analysing samples from children with liver cancer with the intention of making them feel special. Samples are very important to move forward the fight against cancer.
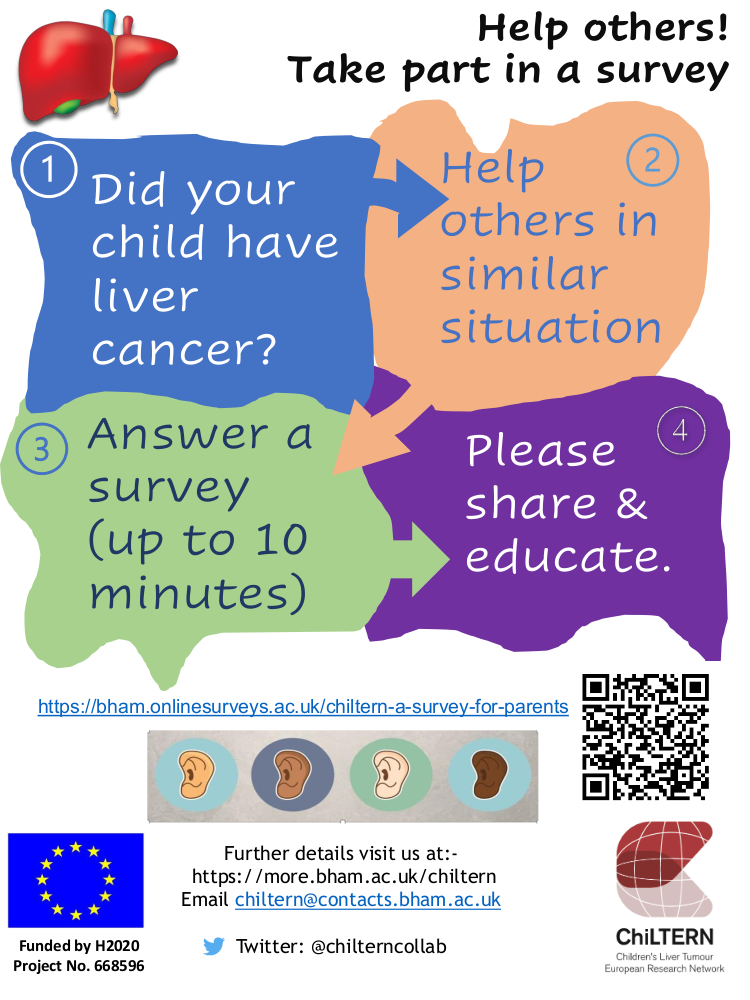
Survey for parents, friends and families with children treated with liver cancer
30 April 2020
https://bham.onlinesurveys.ac.uk/chiltern-a-survey-for-parents
Patient stories
Ollie’s experience
20 Oct 2020

Hi – my name is Ollie and I’m 14 years old. When I was 5.5 months old, I was diagnosed with an Hepatoblastoma. I don’t really remember a thing about my treatment although I do have some memories of visiting Great Ormond Street Hospital. I remember playing with the bead toys in Peppy Brock’s consultation room and I remember throwing fish into a bucket for one of my hearing checks. My mum says that once I got so into building a tower with blocks during one hearing check that I kept on putting more and more blocks on even when they weren’t playing the sounds.
When I was in year 2 of Primary school I got told off in class for talking and I got really upset because I hadn’t heard the teacher say ‘No talking’ I found it hard in the lunch hall because it was so noisy. I couldn’t hear what my friends were saying so sometimes I just nodded and pretended to be able to hear. Sometimes they would then ask me questions about what they’d just said, and I’d have to say, ‘sorry can you say that again – or sorry I didn’t quite hear you.’ This could be embarrassing – not because I couldn’t hear but ‘cause I had pretended to and now I was caught out!
Sometimes at home my Mum asks me to take out the rubbish and I can vaguely make out the words from upstairs but still choose to pretend like she’s said nothing until she calls for the third time – a bit louder and I say “Sorry I didn’t hear you.“ Sometimes not being able to hear can work in your favour!









Richard’s and Philly’s experience
Hello – my name is Philly Simpkin along with my husband Richard we would like to share with you our story about our son Ollie.
Ollie was just like any other baby. He had big podgy cheeks and was always very smiley. When he was 5.5 months old he was lying on the sofa when I noticed a lump protruding just above his nappy line. I stroked his tummy and gave it a prod. It was solid and hard when I pushed it, but Ollie didn’t seem cry or seem to be in any pain in any way, so I wasn’t too worried. When Rich came home from work I showed him and we thought probably that it’d be best to get it checked out by the GP the next morning to be sure.
Our GP examined Ollie the next morning and sent us straight to A+E since in her words ’babies shouldn’t have lumps.’ After much poking and prodding, ultra sounds and consultations I was asked to call my husband because they needed to speak to both of us. They said Ollie had a tumour and the consultant told us to clear our diaries as our lives were about to change considerably. He asked us how we were feeling about this. Being Christians, my husband replied that ‘Though it was surprise to us nothing is a surprise to God.’ so we would trust him for everything that was to come. Amazingly by 7.30pm that same night we were on the Oncology ward at GOSH.
Over the next couple of days after blood tests and MRI scans we were told that Ollie had an Hepatoblastoma. Our son would need to have chemotherapy and part of his liver removed. We were obviously shocked, but with God’s help and the support of a wonderful church family and the remarkable care of our consultant Peppy Brock and the rest of the GOSH oncology team we embarked on this course of treatment.
Ollie had 6 rounds of chemotherapy to reduce to the tumour before surgeons at Great Ormond Street removed it in a 4 and half hour operation. We had been quite cautiously optimistic through everything, but I couldn’t take him down for surgery. Rich had to do that! After a successful operation Ollie had a further 2 rounds of chemo to ‘mop up.’ After 9 difficult months, Ollie was declared cancer free in July 2007. He is, in every way, a normal 14-year-old. He loves playing his Nintendo switch, watching movies and dodging kisses from his Granny. He is kind and mature – very sensitive to how others are feeling and loves hanging out with his mates at church youth group.
Now, we are dealing with the effects of Ollie having so much chemo, at such a high toxicity, at such a young age. One of the chemotherapy drugs that Ollie had during treatment, called Cisplatin, is extremely strong. It’s very effective at shrinking tumours, but it can also lead to side effects like hearing loss.
Thankfully, this has been kept to a minimum for Ollie, but he has Brock Grade 1 Ototoxicity. This means that he finds it hard to hear key consonants at high frequencies like ‘s’ ‘h’ and ‘f’. He has to sit at the front of his class at school and he finds it really hard to hear if there’s a lot of background noise like in the lunch hall or walking down a busy London street, or funnily enough when we say, ‘Ollie, can you take the rubbish out please!’
Fortunately, Ollie’s hearing loss has stabilised for now, but it’s so important that he protects the hearing that he has. It can be tough dealing with his disappointment with not being able to do everything that as a 14-year-old boy he would like to do. When starting secondary school last year, he was disappointed not to be able to learn the drums. But we were advised by his audiology consultant that it was just too much of a risk to his hearing.
By Philly Simpkin
Olaf’s journey
Hello, my name is Iwona and I would like to share my son’s Olaf journey.
Olaf was perfectly growing baby and one day I’ve decided to take him to the walk-in clinic in our health centre as he was not very keen on solid food. For some time we could feel a small lump on his tummy but thought it’s a hernia or muscle. When I mentioned the lump to health visitor she was straight on it, within an hour Olaf had an appointment with GP and in the next 3 hours, we were in Royal Aberdeen Children’s Hospital. The same day Olaf had an ultrasound and blood and we were asked to stay at the hospital that night. I remember when we were waiting to be seen by the doctor my husband asked a question if I think this could be cancer – I denied angrily that is not possible.
The very next morning I’ve been asked when my husband Peter will be able to join me. I said 9.30 am and at that time 2 doctors and nurse came into the room, sat down and said Olaf has liver cancer and they’re 90% sure it’s hepatoblastoma. The whole world went upside down, time has stopped. Olaf got his diagnosis exactly when he was 9 months old, one week before Christmas. In the next couple of days things were going pretty quick, CT, MRI, Hickman’s line, consents to sign, lots of meetings. Olaf diagnosis was Hepatoblastoma pretext 2 and pretty straight treatment 4 rounds of chemotherapy, resection, 2 rounds of clean up chemo. We took a deep breath and concentrated on his treatment. Olaf spent his first Christmas, Hogmanay and his first Birthday at the hospital. After 3 rounds of chemotherapy he had his CT and MRI to see how the tumour is responding to treatment, the news was not too good as the tumour was not shrinking. It has been decided to add another, a stronger drug to which it has responded very well but made Olaf very poorly. We were waiting to finish now all cycles of chemotherapy and wait for resection but in meantime, surgeons confirmed that resection might not be successful due to the location of the tumour and Olaf will need a liver transplant. We went through another shock, what seemed to be simple looking treatment change to a proper ride on a rollercoaster.
After a full week transplant assessment in Birmingham Children’s Hospital, we came back home to Aberdeen to wait for Olaf’s blood cell go back to a normal level. We got a phone call that Olaf is ‘live’ on the transplant list and we need to be ready any time now. We got a phone call about a potential donor, not even 24 hrs after he went live on the transplant list. Scottish Ambulance Service flew us into Birmingham. Unfortunately, the donor’s liver was not suitable. We’ve waited a couple more days at Birmingham for another liver and went back to Aberdeen as there was no suitable liver available. We waited a few more days and got another call. Went to Birmingham again. Olaf has been taken to theatre and a couple of hours later I’ve received the call that surgeons managed to save Olaf’s liver and removed the tumour with clear margins (no cancer cells been left). We were over the moon. Olaf recovered very quickly, we flew back just 5 days after his resection. His Hickman’s line has been removed, Olaf rang the bell announcing finish of the treatment and he went to reemission. We’ve started living a ‘new normal’ life.
The same day at the evening after Olaf attended his first oncology clinic where his blood was taken we got the phone call that his blood needs to be repeated. We went to hospital very next day, another sample was taken only to confirm that his cancer is back. We were devastated, this hit us even more than when he was diagnosed as at this stage you know what your child will have to go through again.
Doctors from Birmingham Children’s Hospital decided to give his liver another chance and after a couple of rounds of chemotherapy (vincristine and irinotecan), they done procedure called microwave ablation (burnt the tumour cells with a probe). The sun was shining again but unfortunately not for long. After 2 months the cancer was back.
We’ve been told there is only one option left – a liver transplant. Olaf went live on the transplant list and again he didn’t have to wait long. Just after a few days, I’ve picked up a phone and we flew to Birmingham. It was a long day of waiting but so worth it. He was taken about 7 pm to the theatre and just after 1 am, I’ve received a call that operation was successful and Olaf is doing well. We were back home just after 2 weeks from transplant. Olaf was making small progress each day, we had to learn a lot, how to tube-fed, how to prepare and administer his medication.
Because of chemotherapy, Olaf lost his high-frequency hearing. He doesn’t wear hearing aids as it’s hard to say now if he needs them (not the easiest patient to work with during an audiology test :0). I think that treatment had also impact on Olaf’s behaviour. When he was 3 and 4 he had a lot of tantrums and a simple thing could cause it. The clinical psychologist helped a lot to deal with it.
Olaf is happy, full of energy 5-year-old boy now. When people find out about his story they cannot believe that he went through so much. He looks and behaves like any other children.





By Iwona Dasko-Rejzner
Cristina’s story
Our son Josemaria (our second child) had congenital liver cancer, and we had to wait 23 days to receive the diagnostic. Why? Because two TAC were needed. Since the first one wasn´t done properly because Josemaria moved.
The second one wasn´t clear enough, because doctors doubted whether it was a vascular tumor or hepatoblastoma. The doctors decided to undertake a biopsy. Unfortunately, the biopsy was an insufficient sample, so a second one had to be done. This time, it was enough. It was a hepatoblastoma.
The hardest moment for us, was right after the first biopsy because the anatomy pathology doctor wrote in the medical report: “vascular tumor?”, with a question mark. Then, I called a friend of mine, who is an anatomical pathologist, and he warned me about the danger of doing a biopsy on a patient, especially a child with a vascular tumor because there high probabilities of death.
I think doctors mustn´t write on their reports diagnostic doubts.
During the treatment (protocol SIOPEL), we were discharged from the hospital several times, which allowed us to disconnect from the hospital and live a normal life.
I think those short periods at home, are extremely helpful for all the family.
Josemaria was 3 months when he underwent surgery. Fortunately thank God it was successful. After surgery, Josemaria had a fever for several days and we didn´t know the cause. It was Christmas time, which meant that the staff of the hospital was reduced and his surgeon wasn´t there. Fortunately, his oncologist requested an ecografyscess (echograph) which showed that an abscess had developed as a complication secondary to the surgical intervention.
I would recommend the surgeons should inform the oncologist about possible complications after surgery.
Another crucial aspect is how the staff deals with patients and their families. They are not aware of the impact a minimal gesture can have on people going through these kinds of tough situations. For example, asking for a pillow, and receiving not only the pillow but also a smile.
Josemaria is 9 years old now. He is in great health, thank God!!!
By Cristina Ogáyar
ChiLTERN Public Advisory Group
November 2019
The advisory group met in London for the first time in November 2019. We are currently a small group made up of clinical trial team members, a doctor leading on liver cancer research, parents and survivors of childhood liver cancer and myself a retired consultant paediatric oncologist. Our aim is to explore the lived experience, views and opinions of parents and survivors to enable improvements to be made in future clinical trial design and information sharing. We plan to meet again in February 2020 in the UK and then to hold an all-day meeting at the next ChiLTERN conference in Munich in March/April 2020.
Our aims are to prepare, administer and analyse a simple online questionnaire which will be made available to parents, patients and survivors of the current Paediatric Hepatic International Treatment Trial known as PHITT. The idea being to improve clinical trial design and information sharing in the future. To prepare and distribute information for schools receiving a child back after diagnosis, perhaps still going through treatment or having already finished treatment. To explore the opportunities offered by social media to share information, support others going through the same experience and increase the general understanding of living with and after liver cancer treatment.

Peppy Brock
Chair ChiLTERN PAG
February 2020
ChiLTERN Public Advisory Group held its second meeting in Birmingham earlier this month. Since we last met, we have now grown from five parents/patients to ten members, within a space of two months. Really looking forward to welcoming new parents and patients from Europe next month! If you are interested, please contact n.mohdtaib@bham.ac.uk

Bruce Morland recently presented to the 2020 Hepatoblastoma Community Group in February 2020 about the latest activities by ChiLTERN Public Advisory Group.
ChiLTERN Public Advisory Group has set up an independent Facebook account to reach out to the wider community, both within the UK and Europe as well as internationally. If you would like to join us, please our parent member, Mr Jawwad Tanvir who is contactable via j.tanvir@icloud.com
